Understanding the complex interplay between the central nervous system and the immune system, and its role in age-related conditions such as Alzheimer’s, Parkinson’s, and arthritis, is crucial for developing innovative therapies. This perspective was a key focus for speakers at MIT’s symposium, “The Neuro-Immune Axis and the Aging Brain,” held on September 18.

Speaking to an audience of over 450 registrants, Picower Professor Li-Huei Tsai, who directs The Picower Institute for Learning and Memory and MIT’s Aging Brain Initiative (ABI), underscored the substantial progress made over the past decade in comprehending how adaptive and innate immune systems influence the development of neurodegenerative disorders. Professor Tsai highlighted that the event’s speakers would explore the intricate relationship between the neuro-immune axis and its role in brain health and disease. Their collective research, she noted, points towards the exciting potential of immunology-informed therapies to slow or even prevent neurodegeneration and age-related cognitive decline.

Dr. Michal Schwartz, a distinguished researcher from Israel’s Weizmann Institute, has dedicated decades to understanding the complex interplay within the neuro-immune system. Her groundbreaking work has demonstrated that immune cells are vital not only for brain repair but also for supporting critical functions, including neural plasticity—the brain’s inherent ability to adapt and process new information.
However, Schwartz’s laboratory also uncovered a concerning aspect: the onset of an immune signaling cascade linked to aging that can detrimentally impact cognitive function. This crucial discovery led her team to investigate and develop corrective immunotherapies. These treatments are designed to bolster the brain’s immune defense against Alzheimer’s disease by rejuvenating the brain’s own microglia immune cells and enlisting the aid of peripheral immune cells known as macrophages. The potential therapy is now advancing to clinical trials, with Dr. Schwartz serving as chief science officer for ImmunoBrain.
Recent research presented by scientist Tsai, a collaboration between her lab and computer science professor Manolis Kellis, offers a new perspective on Alzheimer’s disease. Their work indicates that many genes linked to Alzheimer’s are most prominently expressed in microglia. This genetic expression profile, Tsai explained, bears a stronger resemblance to autoimmune disorders than to many psychiatric conditions, where disease-associated gene activity typically peaks in neurons. The study further revealed that throughout the course of the disease, microglia become “exhausted,” losing their distinct cellular identity and transitioning into a harmful inflammatory state.
Dr. Tsai asserts that genetic predisposition, epigenomic instability, and the exhaustion of microglia are central to the pathology of Alzheimer’s disease. Her laboratory is also actively exploring the potential contribution of immune T cells, which are recruited by microglia, to the overall progression of the neurodegenerative condition.
The human physical form and its central cognitive organ.
The neuro-immune axis establishes a comprehensive connection, linking not only the nervous and immune systems but also bridging the brain with the entire body, holding profound implications for the aging process. Experts underscored the vagus nerve as a pivotal pathway within this system, noting its crucial role as it extends directly from the brain to the body’s major organs.
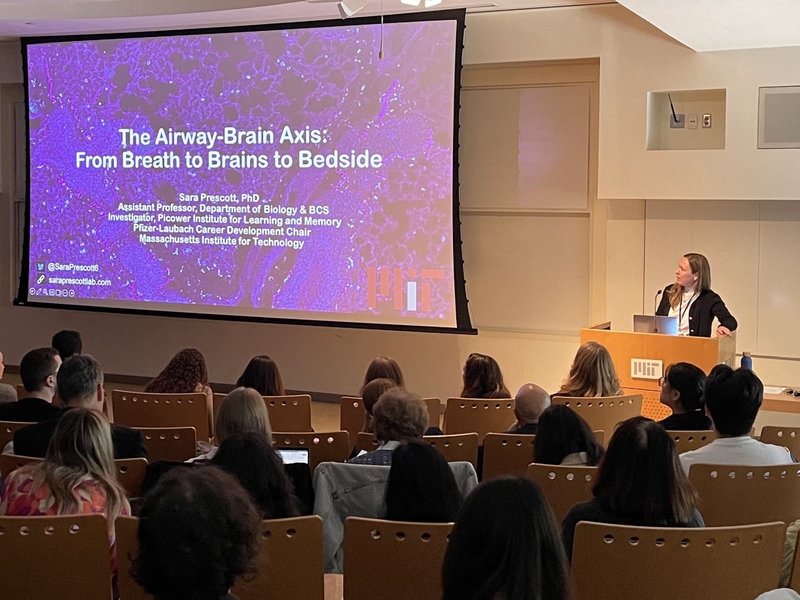
Dr. Sara Prescott, an investigator at the Picower Institute and an MIT assistant professor of biology, has presented compelling evidence suggesting a critical role for brain-vagus nerve communication within the body’s airways in safeguarding respiratory tissues. Given that humans breathe approximately 20,000 times daily, airways face constant environmental challenges. Prescott’s lab and others are uncovering how the nervous system directly engages immune pathways to orchestrate physiological defensive responses.
However, Prescott highlighted a concerning decline in vagal reflexes as individuals age, a factor that heightens susceptibility to infections. In response, her team is now utilizing mouse models to comprehensively study airway-to-brain neurons across the entire lifespan, aiming to better understand the age-related transformations in these vital communication pathways.
Research from Caltech Professor Sarkis Mazmanian’s laboratory is illuminating a critical connection between the gut microbiome and Parkinson’s disease (PD). Professor Mazmanian’s presentation detailed how the microbiome contributes to the alpha-synuclein protein pathology and motor deficits observed in mouse models. The lab’s central hypothesis posits that bacterial amyloid proteins within the gut could initiate the aggregation of alpha-synuclein, with this pathology potentially migrating to the brain via the vagus nerve.
Building on these insights, the lab has advanced two therapeutic strategies. The first involves administering a high-fiber diet to alpha-synuclein overexpressing mice. This dietary approach aims to boost gut short-chain fatty acid levels, which subsequently modulate microglia activity in the brain. Data presented indicated that this high-fiber regimen successfully alleviated motor dysfunction, corrected microglia activity, and diminished protein pathology. The second intervention is a pharmaceutical agent designed to disrupt bacterial amyloid proteins in the gut. This drug demonstrated the ability to prevent alpha-synuclein formation in the mouse brain and ameliorate PD-like symptoms. These promising results are currently awaiting peer-reviewed publication.
Kevin Tracey, a professor at Hofstra University and Northwell Health, recently offered insights into the vital role of the vagus nerve, detailing its connection to the spleen. He explained how nerve impulses regulate the immune system’s emission of signaling molecules, or cytokines. Tracey emphasized that an uncontrolled surge in these cytokines can be damaging, leading to autoimmune conditions like rheumatoid arthritis. He then unveiled a significant medical advancement: a newly U.S. Food and Drug Administration-approved, pill-sized neck implant designed to stimulate the vagus nerve. This innovative device provides relief for patients with severe forms of rheumatoid arthritis, notably without requiring the suppression of their immune system.
The intricate frontier of the human brain.
Recent discussions among experts have underscored the significant potential for understanding neuro-immune interactions, particularly in the context of aging and various diseases. A key focus was placed on the “border regions” where the brain’s distinct immune system meets and interacts with the body’s broader immune network. These critical interfaces include the meninges, the protective membranes surrounding the brain; the choroid plexus, situated near the brain’s internal ventricles (fluid-filled spaces); and the crucial junction where brain cells connect with the circulatory system.
Professor Beth Stevens of Harvard Medical School and Boston Children’s Hospital recently detailed new research exploring how the brain’s immune cells adapt to the day-night cycle, building on established links between circadian rhythm disruptions and Alzheimer’s disease.
The findings, from a project spearheaded by newly minted PhD Helena Barr, highlight that “border-associated macrophages”—durable immune cells situated at the brain’s periphery—exhibit distinct circadian rhythms in both their gene expression and functional activity.
Stevens elaborated that these cells are biologically programmed by the circadian clock to heighten their “eating” activity—a process critical for cellular waste removal—during the brain’s natural rest phase. This function is thought to assist in clearing draining materials from the brain, including amyloid-beta peptides associated with Alzheimer’s disease.
Consequently, Stevens posits that interruptions to these circadian rhythms, such as those caused by aging or consistent night-shift work, may precipitate disease onset by compromising the brain’s finely tuned immune-mediated “clean-up” operations at its borders.
Washington University Professor Marco Colonna, speaking after Stevens, detailed the embryonic development of various macrophage types, including border macrophages and microglia. He elucidated the distinct gene-expression programs that guide their differentiation into specialized forms. Colonna highlighted one particular gene essential for border macrophages along the brain’s vasculature, which plays a crucial role in regulating the waste-clearing cerebrospinal fluid (CSF) flow, a mechanism Stevens had also addressed. Disabling this specific gene was also shown to impair blood flow. Importantly, Colonna’s laboratory has discovered that certain versions of the gene may offer some protection against Alzheimer’s disease, suggesting that regulating its expression could become a promising therapeutic strategy.
Dr. Jonathan Kipnis, a colleague of Colonna at Washington University and a former student of Schwartz, has highlighted the integral function of macrophages positioned at the intricate border separating brain tissue from the perivascular spaces that facilitate cerebrospinal fluid (CSF) flow. His laboratory’s 2022 research revealed that these specific macrophages are active regulators of CSF circulation. The studies further indicated that the removal of these macrophages in mice resulted in the buildup of proteins linked to Alzheimer’s disease. Kipnis’s team is continuing to explore the various roles these distinctive border macrophages might play in disease progression. Separately, his research also examines the contribution of the skull’s bone marrow to the brain’s immune cell population and its potential involvement in neurodegeneration.
Harvard Medical School Professor Isaac Chiu recently emphasized the direct involvement of neurons in their own immune defense, moving beyond discussions focused solely on distant organs or brain borders. In a presentation, Chiu explained that neurons actively sense pathogens and, upon cell death, generate inflammation signals. He also highlighted a key molecule central to this latter process, which is widely expressed among neurons throughout the brain.
Recent discussions have underscored a significant shift in understanding and potentially treating age-related nervous system diseases. Experts demonstrated that a more comprehensive approach, one that considers not only nerve cells but also their immune system partners, is leading to improved insights and therapeutic possibilities. This integrated perspective holds true regardless of whether the focus is on the brain’s internal workings, its protective borders, or the nervous system’s function throughout the entire body.