In a remarkable stride for assistive technology, a pairing of surgically implanted microchips and augmented-reality glasses is now enabling some individuals who have experienced significant sight loss to regain their ability to read.
New research offers encouraging prospects for individuals affected by vision loss due to age-related macular degeneration (AMD). A preliminary clinical trial, detailed in a study published Monday, October 20th, in The New England Journal of Medicine, revealed that approximately 80% of participants experienced a notable improvement, regaining the ability to read letters and words a year after receiving treatment.
This groundbreaking advancement marks “a new era” in the history of artificial vision, according to Mahi Muqit, an ophthalmologist at University College London and the Moorfields Eye Hospital in the U.K., and a co-author of the study. Muqit emphasized that, for the first time ever, blind patients are now achieving “meaningful central vision restoration”—a feat previously deemed unattainable.
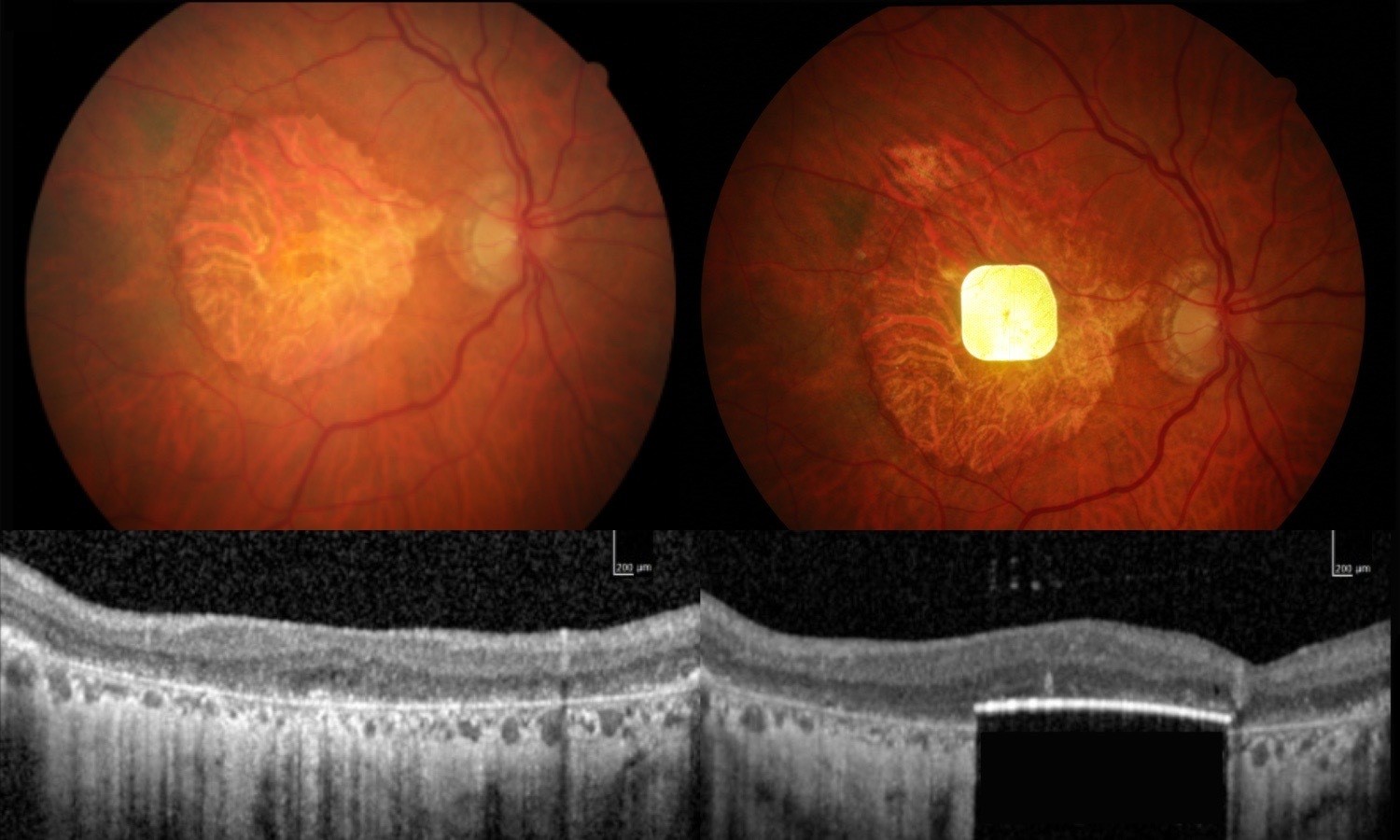
Age-related Macular Degeneration (AMD) stands as the leading cause of blindness among adults over the age of 65. This condition critically impacts the macula, the central region of the retina, progressively eroding central vision. For those with advanced AMD, a destructive process termed geographic atrophy causes extensive damage to retinal cells, which can ultimately lead to total blindness in the affected eye. This severe manifestation of the disease currently afflicts an estimated 5 million people globally.
Sheila Irvine, a participant in the study diagnosed with Age-related Macular Degeneration (AMD), offered a stark description of her vision before receiving the implant. In a statement, she recounted her sight as being obscured by what felt like “two black discs,” compounded by significant distortion in her peripheral vision.
In a pilot clinical trial, 38 European patients grappling with Age-related Macular Degeneration (AMD) have received a groundbreaking electronic retinal implant. The procedure involved surgically placing a miniature electronic chip beneath the center of the retina, specifically in areas where crucial cells had deteriorated. This innovative implant wirelessly communicates with a pair of augmented-reality glasses, which are then connected to a compact computing device designed to be worn by the patient on their waistband.
The Photovoltaic Retina Implant Microarray, or PRIMA system, employs a sophisticated process to facilitate visual interpretation. This technology begins with a video camera integrated into a pair of specialized glasses, which captures images of text. The glasses then project this visual information as infrared light directly onto a microchip surgically implanted in the retina. The implant’s critical function is to convert this infrared light into electrical signals, which the brain subsequently processes and perceives as vision.
Irvine described a profoundly altered visual experience, stating that the initial recognition of individual letters brought immense excitement. He acknowledged the considerable challenge of relearning to read but emphasized that sustained effort directly correlates with improved comprehension.
Participants in the study dedicated several months to intensive training, learning to read proficiently using the innovative device. Beyond formal instruction, researchers encouraged patients to creatively integrate the technology into their daily lives. Illustrating its versatility, one participant, Irvine, utilized the device to complete crossword puzzles, while another successfully navigated the complex Paris Metro system. Furthermore, the device incorporates a crucial zoom function on its camera, enabling users to effortlessly read fine-print text, such as details found on prescription labels.
Dr. Demetrios Vavvas, director of the retina service at Mass Eye and Ear, who was not involved in the PRIMA system study, has highlighted key limitations of the device. Currently, the system can only restore black and white vision, lacking the capacity for color or grayscale perception. This fundamental restriction means it cannot be utilized for intricate visual tasks such as facial recognition. Additionally, questions persist regarding the device’s long-term effectiveness, with its sustained performance over multiple years of use yet to be determined.
Speaking to NBC, Vavvas conveyed that the device holds significant future promise. He suggested that as successive versions demonstrate enhanced capabilities, the technology could ultimately deliver a crucial solution for a specific patient population.