A groundbreaking new study suggests that the mRNA-based COVID-19 vaccines, credited with saving an estimated 2.5 million lives globally during the pandemic, may hold a surprising key to fighting cancer by stimulating the immune system. This significant finding, published in the journal *Nature*, represents a pivotal takeaway from research conducted by the study’s authors.
In 2016, a research team led by pediatric oncologist Elias Sayour made a pivotal discovery while developing mRNA vaccines for brain tumor patients. They found that messenger RNA (mRNA) possesses the remarkable ability to program the immune system to target and destroy tumors, a capability observed even when the mRNA was not directly related to cancer itself.
A significant new hypothesis proposes that mRNA vaccines, specifically engineered to combat the SARS-CoV-2 virus and its resulting COVID-19 disease, could unexpectedly demonstrate efficacy against cancerous tumors.
Researchers have analyzed clinical outcomes for over 1,000 patients diagnosed with advanced melanoma and lung cancer. All participants received immune checkpoint inhibitors, a potent form of immunotherapy.
This widely adopted medical approach leverages the body’s own defenses to combat malignancy. Its efficacy stems from blocking a protein synthesized by tumor cells. Ordinarily, this protein deactivates immune cells, but by inhibiting its action, the treatment ensures the immune system can persistently target and eliminate cancerous growths.
New research indicates a striking correlation between receiving an mRNA-based COVID-19 vaccine (Pfizer or Moderna) and improved survival rates for cancer patients undergoing immunotherapy. Patients who were vaccinated within 100 days of commencing immunotherapy were more than twice as likely to be alive three years later compared to those who did not receive either vaccine.
The benefits were particularly significant for individuals battling tumors typically unresponsive to immunotherapy, where a nearly fivefold improvement in three-year overall survival was observed. This robust link between mRNA vaccination and enhanced survival remained consistent, even after controlling for various influencing factors such as disease severity and co-existing medical conditions.
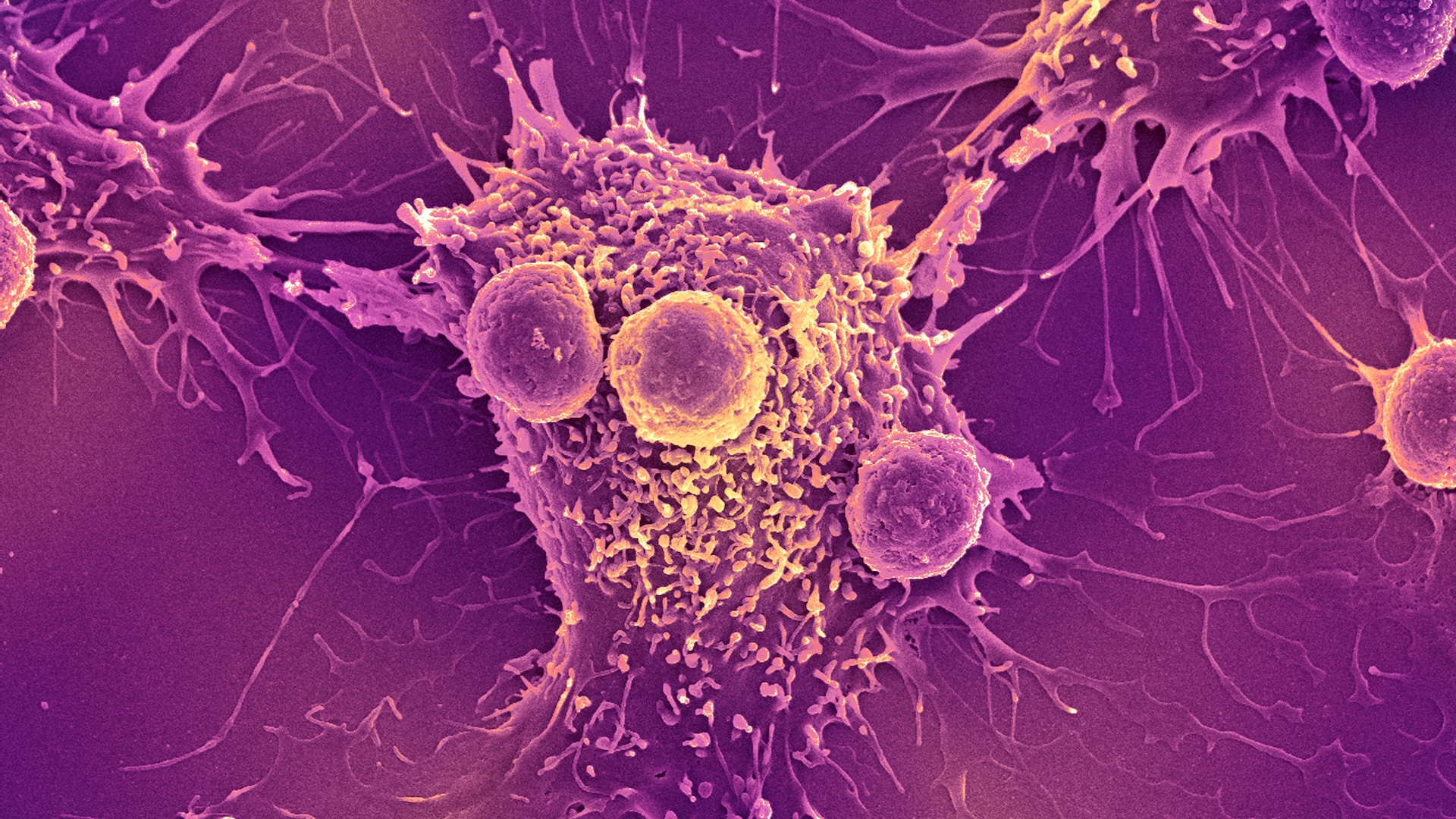
In studies utilizing animal models, researchers have uncovered a fascinating mechanism: COVID-19 mRNA vaccines appear to act as a crucial alarm, galvanizing the body’s immune system. This activation prompts immune cells to both identify and eradicate tumor cells, while simultaneously overcoming cancer’s notorious ability to disarm these vital defenses. When strategically combined with immune checkpoint inhibitors, this powerful duo effectively orchestrates the full mobilization of the immune system, unleashing its potent power to destroy cancer cells.
The past decade has witnessed a profound transformation in cancer treatment, largely spearheaded by immunotherapy, particularly immune checkpoint inhibitors. These innovative therapies have delivered life-saving results, achieving cures in numerous patients previously considered beyond hope.
Yet, their impact is not universal. A persistent challenge lies in “cold” tumors, which expertly elude immune detection, rendering these potent treatments ineffective for affected individuals.
New research suggests that mRNA vaccines may hold the key to activating the immune system against “cold” tumors, effectively transforming them into “hot,” immune-responsive cancers. Should these preliminary findings be validated in upcoming clinical trials, scientists are hopeful that this widely available and low-cost intervention could significantly broaden the reach of immunotherapy, offering new treatment avenues to millions of patients who currently do not benefit from this type of therapy.
Unlike conventional vaccines, which are administered to prevent infectious diseases, therapeutic cancer vaccines serve a fundamentally different purpose. These innovative treatments are designed not to prevent illness, but rather to educate and strengthen the immune systems of cancer patients, enabling them to more effectively recognize and combat existing tumors.
The global scientific community is intensely focused on advancing personalized mRNA vaccines for cancer patients. This innovative therapeutic strategy involves taking a small sample from a patient’s tumor, which is then analyzed using advanced machine learning algorithms. The primary goal is to precisely identify specific proteins within the tumor that would serve as the most effective targets for a customized vaccine. However, this highly tailored approach currently faces significant hurdles, primarily its substantial cost and the inherent complexities associated with its manufacturing processes.
Unlike personalized cancer therapies, COVID-19 mRNA vaccines offer distinct advantages. They do not require individual tailoring, are already broadly accessible globally at minimal or no cost, and can be administered flexibly at any point during a patient’s treatment regimen.
Crucially, our research demonstrates that these widely available vaccines possess substantial anti-tumor effects. This groundbreaking finding sparks significant hope, suggesting that the anti-cancer potential of mRNA vaccine technology could soon be extended to a far wider patient population.
To further this crucial objective, a nationwide clinical trial is being prepared to evaluate a specific treatment strategy for individuals diagnosed with lung cancer. The study will involve patients currently receiving an immune checkpoint inhibitor and will randomly assign them to one of two groups: either receiving a COVID-19 mRNA vaccine concurrently with their treatment or continuing treatment without immediate vaccine administration.
A new study is underway to determine if COVID-19 mRNA vaccines should become a standard part of treatment protocols for patients receiving immune checkpoint inhibitors. The ultimate aspiration is for this approach to significantly benefit a wide range of individuals undergoing immune therapy, particularly those who currently face a scarcity of effective treatment options.
A groundbreaking innovation, initially forged during a global pandemic, is now emerging as a potent new weapon in the battle against cancer. This transformative approach promises to rapidly expand the reach of existing cancer treatments to millions worldwide. By strategically repurposing a common vaccine, scientists aim to extend the life-saving advantages of immunotherapy to patients who, until now, have had limited options.
This article, an edited version of a piece originally published by The Conversation, is made available here under a Creative Commons license.