The very genesis of cellular life on Earth approximately 3.8 billion years ago was met by the inherent presence of viruses. Since that ancient epoch, viruses have relentlessly engineered methods to infiltrate cells, driving cells, in turn, to evolve intricate defenses against these invasions. This ceaseless evolutionary interplay, a profound biological arms race between pathogen and host, ultimately forged the sophisticated immune system that protects organisms today.
The immune system’s fundamental role involves distinguishing between the body’s own components (“self”) and foreign substances (“nonself”). This critical identification process enables it to eliminate external threats, such as viruses, protecting overall health. However, this same inherent ability to recognize and respond to foreign materials also directly influences the effectiveness of introduced substances, including various medications.
Researchers are actively pursuing innovative strategies to optimize drug delivery, with a primary focus on ensuring therapeutic agents reach their intended disease sites within the body before being eliminated or degraded. One promising method involves encapsulating medications within nanoparticles – microscopic carriers small enough to be readily absorbed by cells.
While these nanoscale materials inherently provoke an immune response designed to clear them from the system, scientists have made a compelling discovery: this very biological reaction could potentially be leveraged to significantly enhance the efficacy of cancer treatments.
The immune system serves a dual purpose, not only identifying and neutralizing pathogens but also actively responding to physical tissue damage. This latter function frequently presents as inflammation, a reaction commonly observed as redness and swelling when medications are introduced into the body via injection.
While the body’s inflammatory response to drug administration is typically minor, the potential for a prolonged reaction significantly escalates when medications are delivered slowly over an extended period. This is often observed in chemotherapy infusions, which can span an hour or more. To counteract this, some patients are prescribed anti-inflammatory medications before their infusion, a measure designed to diminish the risk of an adverse immune response during the treatment course.
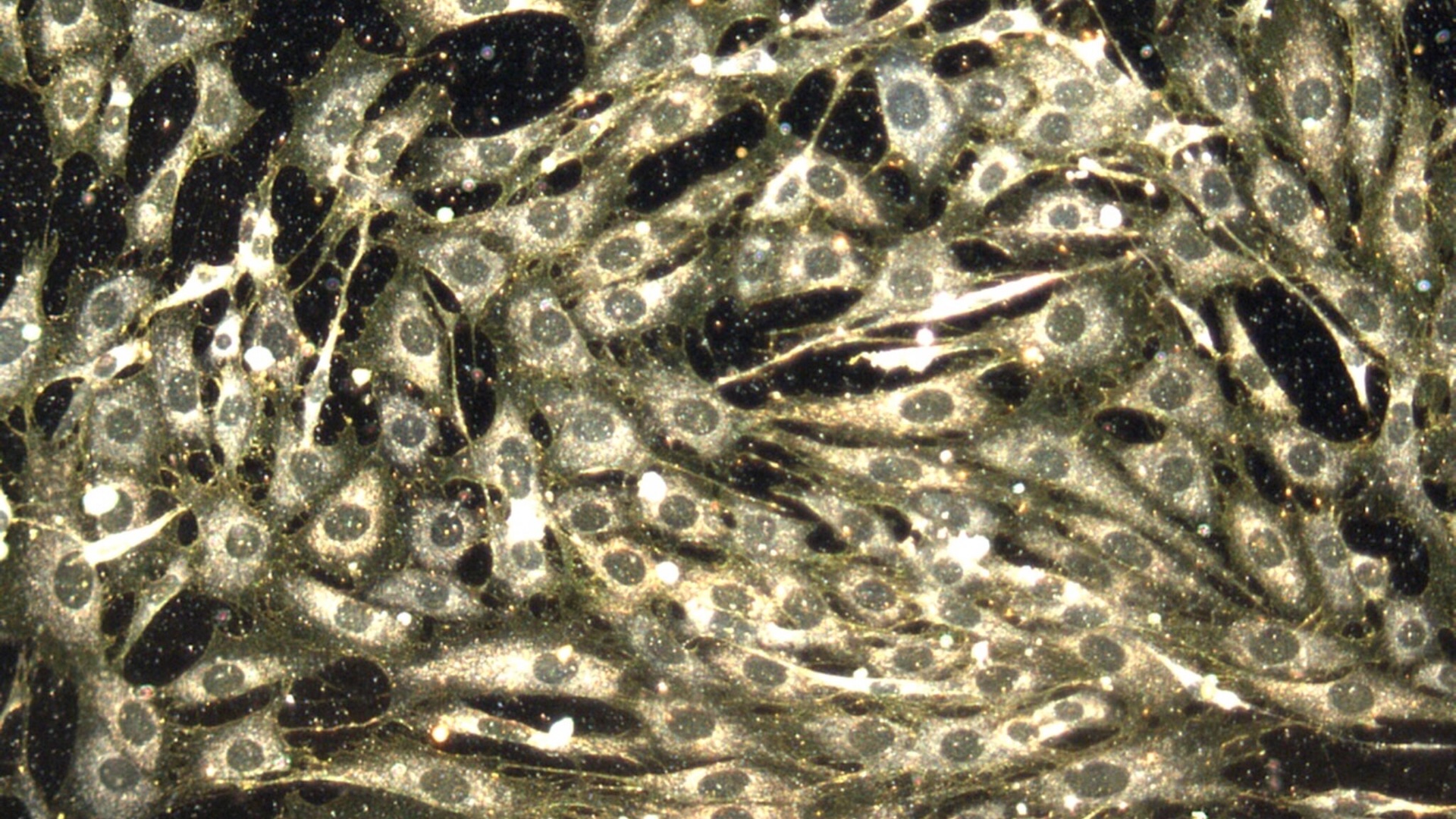
Nanoparticles represent a groundbreaking advancement in pharmaceutical delivery. These innovative materials, which can be engineered from components like lipids, proteins, or even gold, offer a significant advantage due to their minute dimensions. Typically measuring just 10-thousandths of a millimeter in diameter, their exceptionally small size allows diseased cells to readily absorb them. Consequently, when loaded with therapeutic agents, these nanoparticles function as a highly effective and targeted system for drug administration.
Despite their minute size, nanoparticles possess an impressive capacity to encapsulate numerous drug molecules, enabling them to deliver a potent therapeutic payload directly into target cells. These versatile carriers are also capable of transporting genetic material, including DNA and RNA-based drugs. A prominent example of this technology’s application is the COVID-19 vaccine, which utilizes nanoparticles constructed from modified fat molecules. These nanoparticles deliver messenger RNA (mRNA) that educates the immune system, teaching it to defend against COVID-19 infection.
Upon injection, nanoparticles are identified by the body’s innate immune system as foreign objects. This recognition can prompt an initial inflammatory reaction in some patients as the immune system mobilizes to neutralize these particles.
The pivotal question remains: Can this reaction be harnessed to fundamentally enhance treatment efficacy?
A University of Colorado laboratory has dedicated three decades to extensively researching how nanoparticles facilitate drug delivery. More recently, their focus has narrowed to understanding the innate immune system’s response to injected nanoparticles. While this immune reaction is generally perceived as a drawback, the team is now investigating its potential to enhance therapeutic outcomes.
A 2022 study investigating the interaction of nanoparticles with the immune systems of mice has uncovered a significant finding. Researchers observed that an initial administration of drug-carrying nanoparticles triggers an innate immune response. This response subsequently diminishes the effectiveness of a second dose, particularly if administered within days, by accelerating the clearance of the drug from the body. This reaction parallels the natural phenomenon where an initial viral infection provides a short-term protective response against a subsequent viral exposure.
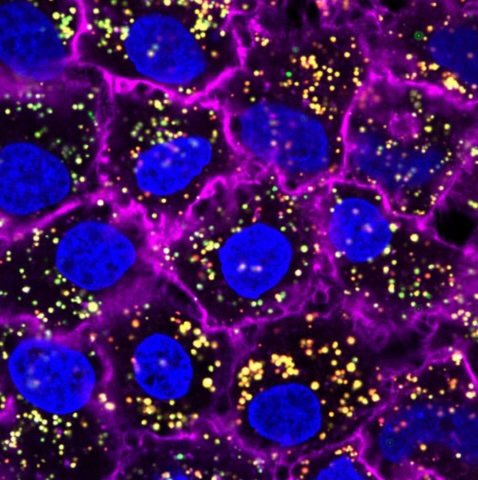
A vital component of the body’s defense against infection involves the production of a protein known as interferon lambda. This molecule actively disrupts the viral replication cycle by preventing pathogens from infiltrating various tissues throughout the body. Notably, interferon lambda has previously been explored by researchers as a potential antiviral drug for the treatment of COVID-19.
An initial administration of nanoparticles triggers the production of interferon lambda, which has been observed to limit the subsequent dose’s capacity for drug delivery to healthy tissues. However, this immune response did not hinder the nanoparticles’ ability to access tumors. Researchers suggest this selective targeting might be attributed to the inherent capacity of tumors to impair the body’s immune defenses.
Conventional cancer treatment utilizes chemotherapy drugs to eliminate tumors. However, these powerful medications are also toxic to healthy cells, frequently leading to patient side effects such as hair loss, gastrointestinal problems, and skin rashes. A promising approach involves using nanoparticles for targeted cancer drug delivery, which could significantly reduce these adverse reactions. Furthermore, combining nanoparticles with interferon lambda may extend the drug’s duration in the body, ensuring sufficient time for its full therapeutic effects to manifest.
A research team is investigating whether directly injecting interferon lambda ahead of nanoparticle-delivered chemotherapy could significantly reduce drug exposure in healthy tissues while simultaneously concentrating it within tumors.
Initial trials on mice with colon cancer have yielded encouraging results. All subjects that received interferon lambda demonstrated increased survival times and experienced reduced weight loss. Further understanding of the biological mechanisms behind these effects is crucial, as it could eventually lead to testing this innovative cancer treatment approach in human patients.
Scientists continue to face a substantial challenge in engineering nanoparticles to infiltrate cells with the same efficiency as viruses. Nevertheless, a promising new approach seeks to leverage an ancient immune response, one that evolved approximately a billion years ago specifically to combat viral infections. Researchers anticipate this strategy could significantly reduce the toxic side effects associated with current treatments while simultaneously enhancing their overall effectiveness.
This edited piece was originally published by The Conversation and is presented here under a Creative Commons license.